Diabetic Foot Ulcers – A critical problem in Diabetes Patients
Diabetes can cause a variety of complications, many of which can be fatal if not identified and treated promptly. Diabetic Foot problem or Diabetic foot Ulcers a common problem in Diabetes patient .
In general, you can reduce your risk of diabetes-related complications by maintaining a healthy blood sugar level and visiting your doctor for regular checkups.
You can also reduce your chances of developing foot problems by regularly inspecting your feet. If problems do arise, you will be more likely to notice them right away and receive appropriate treatment. Building good foot care habits may take time and effort, but it is an important part of diabetes management.
This article will go over the foot-related complications that can occur in diabetics, as well as guidelines for good foot care and ways to reduce your risk of developing these issues.
RISK FACTORS – Diabetic Foot Problem
Uncontrolled diabetes can lead to foot complications over time.
Past foot ulcer — Even if a foot ulcer heals completely, you are at an increased risk of developing ulcers in the future.

Nerve Damage — High blood sugar levels can damage the nerves that carry sensation over time; this nerve damage is referred to as “diabetic neuropathy.” Because people with neuropathy may lose their ability to feel pain, they are more likely to injure their feet; even minor injuries can quickly become serious if they go unnoticed. Nerve damage can also cause foot deformities by weakening specific foot muscles.

Foot Deformity — Shape abnormalities in the toes, arches, or bottoms of the feet can increase the risk of complications.

Poor Circulation — Long-term high blood sugar levels can damage blood vessels, reducing blood flow to the feet. Poor circulation can cause skin deterioration, contribute to the formation of foot ulcers, and impede wound healing. Some bacteria and fungi thrive on high blood sugar levels; if a wound becomes infected, this can break down the skin and worsen ulcers.

Deep skin and bone infections are more serious complications. Gangrene (tissue decay and death) is a serious complication that may necessitate amputation. Approximately 5% of diabetics will eventually require amputation of a toe or foot. However, in most cases, this can be avoided by controlling blood sugar levels and committing to daily foot care approaching to a Best Vascular Surgeon in time if occurs.
FOOT EXAMINATIONS – Regular foot exams to check for problems or changes are an important part of diabetes management.
Self-examinations — It is critical to examine your feet every day. This includes paying close attention to all parts of your feet, especially the area between your toes. Examine your skin for broken skin, ulcers, blisters, areas of increased warmth or redness, or changes in callus formation; Immediately approach to a expert for Diabetic foot treatment by a vascular surgeon .
Clinical exams — During routine medical visits, your doctor will examine the blood flow and sensation in your feet. The frequency of these clinical examinations will be determined by the type of diabetes you have:
Annual foot exams for people with type 1 diabetes should begin five years after diagnosis.
Annual foot exams should begin at the time of diagnosis in people with type 2 diabetes.
During a foot exam, your doctor will look for signs of poor circulation, nerve damage, skin changes, and deformities. They will also inquire about any foot problems you have noticed. An exam can detect decreased or absent reflexes, as well as a decreased ability to sense pressure, vibration, pin pricks, and temperature changes.
DIABETES FOOT PROBLEMS PREVENTION
Here are some things you can do to lower your risk of developing foot problems. In addition to controlling your blood sugar, good foot care habits and daily foot checks are essential for avoiding complications.
Importance of blood sugar management — In general, keeping your blood sugar levels as close to your target as possible can reduce your risk of all diabetes-related complications. Managing your blood sugar requires regular doctor visits, healthy diet and lifestyle changes, and taking your medications as prescribed.
Quit smoking — Smoking can aggravate heart and vascular issues as well as reduce circulation to the feet. If you smoke, one of the most important things you can do to improve your health and lower your risk of complications is to quit. While this can be challenging, your health care provider can assist you and provide additional resources for support.
Avoid activities that can cause foot injury — Certain activities increase the risk of foot injury or burns and should be avoided. Walking barefoot (because you might step on something without realizing it), using a heating pad or hot water bottle on your feet, and stepping into a hot bath before testing the temperature are all examples.
Trim your toenails straight across, and avoid cutting them down the sides or too short (figure 1). To prevent the toenail from digging into your skin, use a nail file to remove any sharp edges.
Wash and inspect your feet on a daily basis — Clean your feet with lukewarm water and a mild soap. Dry your feet thoroughly, paying special attention to the spaces between your toes, with a clean, absorbent towel. Apply a hydrating cream or lotion.
Choose your socks and shoes with care — Wear cotton socks that fit loosely and change your socks every day. Choose shoes that are snug but not too tight, with a wide toe box .To avoid consistent pressure on one part of your foot, it may be beneficial to rotate several pairs of comfortable, well-fitting shoes. Ask your provider about customized shoes if you have foot deformities or ulcers; this can reduce your chances of developing foot ulcers in the future. Shoe inserts can also help cushion your steps and relieve pressure on your feet’s soles.
FOOT ULCER TREATMENT
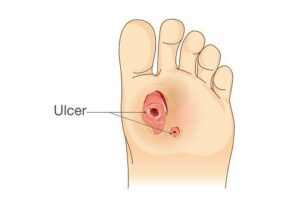
If you develop a foot ulcer, the treatment will be determined by the extent of the damage.
Superficial ulcers — These ulcers affect only the top layers of skin .Your Vascular Surgeon will usually clean the ulcer and remove dead skin and tissue; this is known as “debridement.” Following debridement, the area will be dressed to keep it clean and moist.
More severe ulcers — Ulcers that extend into the deeper layers of the foot, involving muscle and bone usually necessitate hospitalization. Laboratory tests and X-rays may be performed, and intravenous (IV) antibiotics are frequently administered. In addition to debridement to remove dead skin and tissue, surgery to remove infected bone may be required. You may also receive “negative pressure wound therapy,” which entails bandaging the ulcer and using a special vacuum device to help increase blood flow and speed healing.
Some people who have severe foot ulcers and peripheral vascular disease (poor circulation) may need a procedure to restore blood flow to the foot.
While foot problems in diabetes are common and can be serious, its advised to consult the Best doctor for Diabetic foot treatment so to get the Best treatment for your problem.

